How people living with dementia in care homes make and share everyday decisions

ENRICHEnabling Research in Care Homes
GUEST BLOG
How people living with dementia in care homes make and share everyday decisions
Rachel Daly, Professional and Practice Development Facilitator, Dementia UK. Queens Nurse and District Nurse by background with over 20 years’ experience working in and with care homes as a nurse and a family care partner. Tweets as @dementiaventure
In this guest blog Dr Rachel Daly presents six key factors that enable decision-making in care homes for people living with dementia. She discusses the importance of involving people in everyday decisions and recognising a person’s desire and ability to be involved in the decision-making process (regardless of what the decision is).

As a Queens Nurse and District Nurse with 20 years’ experience working in and with care homes, I was always interested in how people living with dementia were involved in the everyday decisions about their life and care. Despite regularly seeing good practice in the care homes I visited, I couldn’t find much research about the importance of everyday decisions for people living with dementia, or how care partners help them to be involved in decisions that matter to them in care homes. While I was looking for research evidence, I stumbled across a funding opportunity for a PhD in dementia care through the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research & Care (CLAHRC) East of England (now called ARC). When I applied I never really thought that would be the start of my PhD journey.
The first step
To help me to understand how people living with dementia in care homes share decisions I explored studies that had already been carried out. By reviewing the work already carried out I found that people living with dementia like to be involved in the decisions that affect their day to day life. I also found that the process of decision-making is as important to people living with dementia as the decision itself. Importantly, staff and family care partners tend to underestimate people’s desire and abilities to be involved in everyday decisions.
My study
I designed the study to reflect the decision-making process and took an inclusive approach. That is, I involved all the people who are important in making everyday decisions in care homes such as, residents living with dementia, care home staff (nurses and care workers) and family care partners from two care homes in England. I observed people making and sharing everyday decisions and made notes about what the decisions were, who (if anyone) helped and how they helped.
I also asked people to tell me about everyday decisions that they made and shared that had gone well. I listened to their stories and was able to identify patterns of how people living with dementia managed decision-making interactions in their care homes. I then invited the residents and their staff and family care partners to share ideas of how everyday shared decision-making could be made even better for people like them.
Findings from the study
The most common decisions that people living with dementia made and shared were about what to eat and drink, where to go, who to spend time with and how to use time (for example; attending organized activities, or deciding when to go to bed). Lots of decisions also included choices about personal hygiene (such as whether to have a wash, a bath or a shower). In total people living with dementia in the care homes were making and sharing up to 20 different decisions in a day.
The creativity of staff and family care partners was often the key to involving residents in decisions about their everyday life. Creative support helped residents retain some control over their everyday lives. Options were sometimes limited to residents known preferences, so that they did not feel overwhelmed by choice. But for others, options were extended. For example, at dinner a resident who did not like any of the available choices decided to have a cheese omelette and another chose to save their hot meal for teatime and had a bacon sandwich for lunch.
Some residents asked lots of different staff and family members for help to make decisions. Finding the right person to help was important to them.
Six Factors That Enable Shared Decision-making
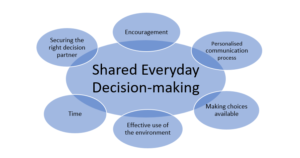
These six factors that helped people living with dementia to be involved in decision-making are explained in more depth in the recommendations table below.
Recommendations
Involving people in everyday decisions about their life and care can help a person feel valued and retain a sense of control.
It is important for staff and family care partners to recognise the person’s desire and ability to be involved in the decision-making process (regardless of what the decision is) and support them to be involved where possible.
| Enabling Factor | How it Helps |
| Encouragement | Motivation and support for a person living with dementia to do something that is considered to be in their best interest, or confidence to try something new.
|
| Communication | Individual approaches that may use multiple senses (for example, using more simple language, breaking down big decisions, pointing to pictures and objects) to help make decision-making easier.
|
| Choices |
Options are; 1) limited to only 2 or 3 choices or 2) expanded with extra information, advice and support to help make the decision. |
| Environment |
Care home routines and environments are changed to help meet more residents preferences and include more people in decisions about their life and care. |
| Decision partner |
The person with dementia chooses who helps them depending on the decision to be made. |
| Time |
Time and space help residents to make decision when they are most able and support to make ‘in-the-moment’ decisions. |
Conclusion
Everyday decisions are regularly made and shared by people living with dementia in care homes. Each person’s understanding of shared decision-making affects how it works for them and who is involved. Staff and family care partners regularly use a range of factors to support people living with dementia to continue to be involved in everyday decisions.
This blog presents independent research funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research & Care (CLAHRC) East of England, at Cambridgeshire and Peterborough NHS Foundation Trust. The views expressed are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.